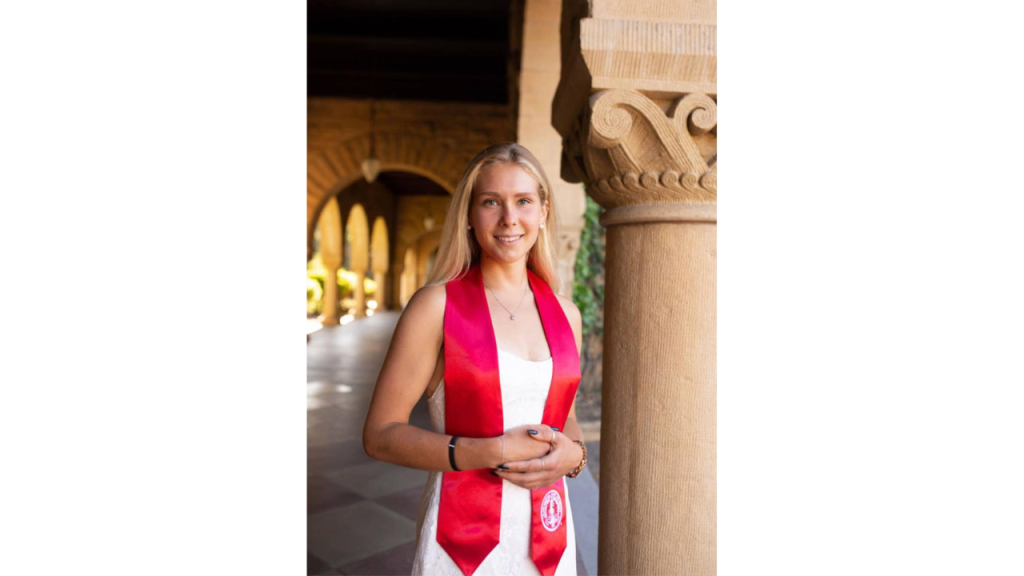
When Maria Shcherbakova walked into an operating room at 19, shadowing a neurosurgeon in Luxembourg, she had no idea the experience would change the course of her life. What she saw was both shocking and mesmerizing: an awake patient undergoing brain surgery. “I told myself: I’m never leaving the OR again,” Shcherbakova recalls.
Now, she is a clinical researcher and software engineer at the Starr Lab at the University of California, San Francisco, co-author on the groundbreaking 2024 Nature Medicine paper, and co-creator of a personalized adaptive deep brain stimulation (aDBS) system. Her specialty is building closed-loop brain-machine interfaces that can read from the brain, respond to pathological activity, and adjust stimulation accordingly.
This aDBS technology is at the center of a shift in how Parkinson’s is treated. One of the major limitations of conventional DBS is its lack of adaptability. These systems apply a continuous pulse throughout the day, regardless of what a patient is doing. Typically used for those who no longer respond well to medication alone, traditional DBS can sometimes result in overstimulation and side effects.
aDBS addresses this challenge by adjusting stimulation levels dynamically, in sync with medication cycles and real-time brain activity, reducing the risk of over-treatment and providing a more stable therapeutic window.
Falling for the Brain
Shcherbakova’s path to neuroscience wasn’t linear. After moving from Russia to Luxembourg at a young age, she eventually landed at Stanford University, where she pursued an individually designed major that combined computer science and bioengineering. Initially drawn to math, she fell in love with computer science: “It had all the logic of math, but it was automatic.”
Stanford’s flexibility allowed her to pursue neuroscience as more than a passion project. She designed a custom curriculum that blended programming, biomechanics, and neurophysiology. Early internships in the IT space gave her a taste of computer science, but from the very first time she set foot in a neuroengineering lab, Maria knew she was there to stay.
By 21, she had joined the UCSF Movement Disorders and Neuromodulation Center in San Francisco, California, a leader in neurology research. Originally planning to work in pharma or pursue medical school, she was drawn to UCSF by the opportunity to help develop implantable brain-computer interfaces capable of not only delivering therapy but also sensing brain signals in real time. “It was bidirectional — the devices could both stimulate and listen,” she recalls. “That’s what excited me most.”
The Algorithms Behind aDBS
Adaptive DBS works by using closed-loop algorithms that adjust stimulation based on the brain’s own rhythms, offering steadier relief than conventional systems. But those algorithms don’t build themselves: they rely on hours of real-world neural data.
“We’ve had 20 patients wearing implanted devices that continuously record brain activity while they go about their day, including hiking, cooking, even skiing,” Maria explains. These devices, developed by Medtronic and refined in partnership with UCSF researchers, don’t just stimulate. They record. “It’s fully invisible. People look at these patients and see nothing out of the ordinary, but we’re collecting neural data from every step.”
Over 500 hours of such real-world recordings helped refine the models. Using these data, Shcherbakova designs algorithms that correlate brain signals with symptom severity and daily behavior. Her models look for neurological “signatures.” These are biomarkers of tremor, rigidity, or other conditions. “If I can reliably detect when a person feels good or bad from a specific brain rhythm, then maybe we can reproduce that effect with stimulation,” she says. “That’s the heart of aDBS.”
The Starr Lab researchers’ methodology combines these long-duration recordings with advanced signal processing and machine learning to identify actionable patterns. These insights are translated into stimulation protocols uploaded wirelessly to the implanted neurostimulators, which continue to learn and adapt over time.
From Prototype to Practice with FDA Greenlight
Once the technical groundwork was in place, the challenge became translating innovation into real-world clinical outcomes. Adaptive DBS has long remained a promising but experimental approach. This status quo changed in February 2025, when the U.S. Food and Drug Administration (FDA) approved adaptive DBS for clinical use.
One of the most transformative features of the approved Medtronic system is its automation of a previously manual process. “Previously, clinicians had to test each electrode contact individually to find the best one. So it was slow, subjective, and depended a lot on experience,” Maria explains. “Now the system can do that automatically.” Using the built-in BrainSense Electrode Identifier, the device stimulates through each contact, records brain activity, and selects the one with the strongest and most reliable signal.
Shcherbakova played a pivotal role in that transition. By embedding patient-tailored algorithms into implanted devices and supporting adjustments based on brain activity, she helped demonstrate that aDBS could offer more consistent symptom control. The technology adapted not only to patient movement, but also to daily fluctuations in medication, mood, and stress. This allows a more personalized therapy.
Expanding the Reach of Brain Stimulation
Shcherbakova is now preparing to take her work a step further: to apply for dual MD/PhD programs. She sees herself as a bridge between two worlds, as someone who understands the clinical needs and the engineering trade-offs. “I bring a rare combination of clinical and technical expertise,” she explains. “I spend a lot of time working directly with patients and doctors. I know what the devices can do and what doctors wish they could do.”
In the near term, she’s finalizing her largest study to date, centered on a specific cortical rhythm that may serve as a reliable biomarker for new therapies. Her team is also exploring high-density cortical arrays that expand neural recording and stimulation capabilities to augment future implantable systems. As interest grows in gamma rhythms alongside beta frequencies, Maria underscores the need for more advanced sensing electrodes and robust artifact rejection.
Long-term, she hopes to expand neuromodulation beyond Parkinson’s to other neurological and psychiatric disorders, making these tools more versatile, compact, cost-effective, less invasive, and easier to access.
But for all the technical progress, Maria is quick to acknowledge that the true challenge in her field lies elsewhere. “The hardest part is the human side,” she says. “In our job, failures don’t just set us back — they affect people who trusted us.” For Shcherbakova, seeing adaptive DBS move from concept to clinic is the most rewarding part of her journey so far. “We’ve proven this therapy can work,” she says. “Now the mission is to make it available to everyone who needs it.”