Medical professionals widely acknowledge that early detection of melanoma is essential for improving patient outcomes, as identifying the disease at its initial stages greatly increases the likelihood of successful treatment and long-term survival.
However, achieving timely and accurate diagnosis presents significant challenges. Early-stage melanomas can be subtle and difficult to distinguish from benign moles or atypical lesions, and conventional histological criteria alone are often insufficient.
Dr. Michael Piepkorn, a seasoned clinical dermatologist, dermatopathologist, and researcher, emphasizes that timely recognition relies heavily on precision in diagnosing melanocytic lesions from skin biopsies. Over decades, the approach to diagnosing melanoma has evolved, moving from broad histological criteria toward more nuanced and technologically supported methods.
The Evolution of Histological Diagnosis
The biopsy diagnosis of melanoma has developed significantly over the last century through algorithms and criteria applied by successive generations of pathologists. These criteria effectively distinguish between the polar extremes of melanocytic growths: benign moles, or nevi, and advanced, potentially fatal melanomas.
Traditional diagnostic approaches have consistently been proven to be reliable for extreme cases. However, their effectiveness is considerably diminished when identifying early-stage melanoma, where the disease is most treatable.
Understanding the Gray Zone
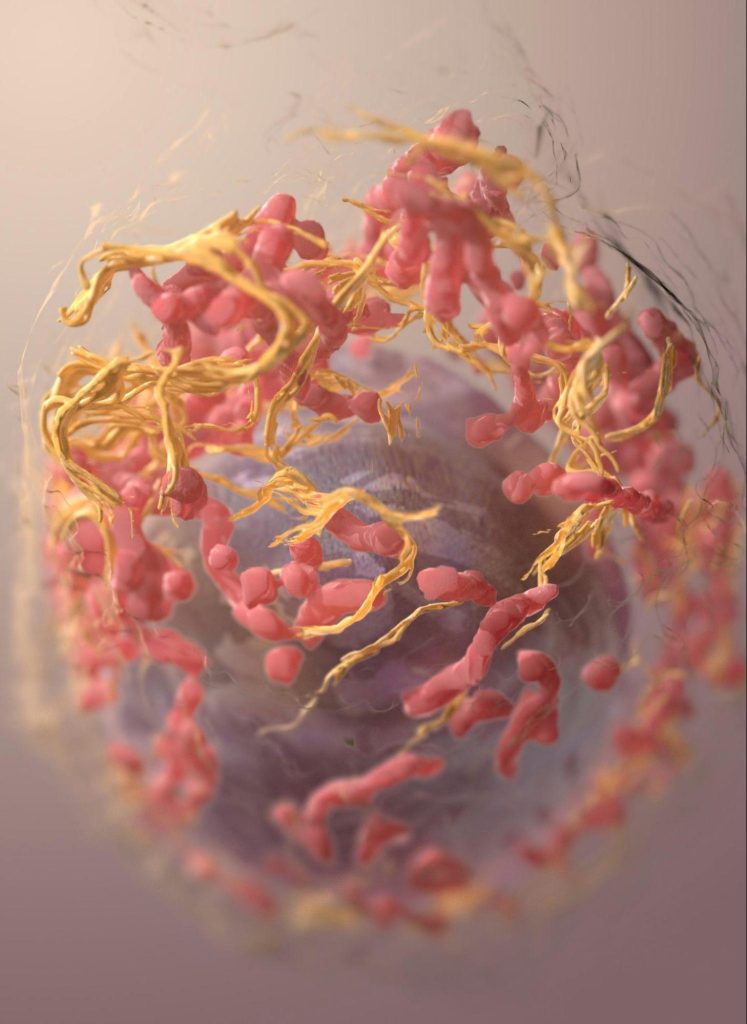
Clinicians have long recognized that melanoma often progresses through a stepwise process. Initial mutations in melanocytic cells may produce benign nevi, some of which acquire further genomic changes, forming atypical or dysplastic moles.
Most of these lesions never become malignant. However, a small subset accumulates additional mutations, developing into fully malignant tumors capable of metastasizing. Conventional histological criteria struggle to reliably differentiate these borderline lesions from early melanoma, creating a diagnostic gray zone that demands more precise techniques.
Enhancing Diagnostic Accuracy with Immunohistochemistry
Dermatopathology has advanced through the integration of ancillary methods, particularly immunohistochemistry (IHC), which employs chemical markers to reveal tumors that may not be fully apparent using traditional criteria. Loss of the tumor suppressor protein p16, for example, can indicate malignant transformation, providing compelling evidence for early melanoma diagnosis.
Other markers, including Melan A and PRAME, offer additional diagnostic utility. Nevertheless, each carries limitations that require careful interpretation.
Dr. Michael Piepkorn’s Contributions
Dr. Piepkorn has played a key role in advancing melanoma diagnostics through research and clinical practice. He contributed to the identification of the familial melanoma gene p16 (CDKN2A) and has published extensively on the accuracy, reproducibility, and technological innovations in dermatopathology.
Dr. Piepkorn’s work at Dermatopathology Northwest in Seattle and at the University of Washington’s pigmented lesion and melanoma clinic underscores his commitment to precise, early detection. Beyond research, he has mentored generations of dermatologists and dermatopathologists, fostering ongoing improvements in melanoma diagnosis.
The Importance of Early Detection
Recognizing melanoma at a curable stage dramatically improves prognosis. Dr. Michael Piepkorn advocates for combining traditional histological criteria with modern techniques, such as IHC, to refine diagnostic precision. This dual approach helps identify malignant lesions before they advance to deeper, life-threatening stages, ultimately saving lives.
Through decades of research, clinical practice, and mentorship, Dr. Michael Piepkorn has reinforced the value of meticulous, evidence-driven diagnosis in dermatopathology. His work demonstrates that advancing early detection requires both scientific rigor and thoughtful application of evolving diagnostic tools, supporting better outcomes for patients at risk of melanoma.